CORNEA
 Corneal blindness is the fourth leading cause of blindness in India. A majority of such patients are children. Treating corneal blindness is possible through cornea transplant. In this treatment, a healthy cornea is transplanted in place of a diseased cornea in entirety through (penetrating keratoplasty) or in part (lamellar keratoplasty). Since artificial corneas are not available, corneas have to be harvested only through eye donation. Our expert cornea specialists offer the most advanced cornea and transplant services . ( Registered Cornea Transplant Centre )
Corneal blindness is the fourth leading cause of blindness in India. A majority of such patients are children. Treating corneal blindness is possible through cornea transplant. In this treatment, a healthy cornea is transplanted in place of a diseased cornea in entirety through (penetrating keratoplasty) or in part (lamellar keratoplasty). Since artificial corneas are not available, corneas have to be harvested only through eye donation. Our expert cornea specialists offer the most advanced cornea and transplant services . ( Registered Cornea Transplant Centre )
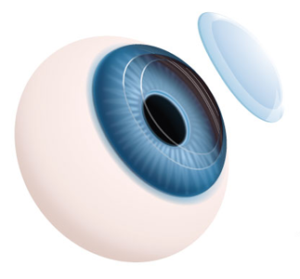
The cornea is the eye’s outermost layer. It is the clear, dome-shaped surface that covers the front of the eye. It is responsible for more than 2/3rd of the eye’s focusing power. Unlike most tissues in the body, the cornea contains no blood vessels to nourish or protect it against infection. Instead, the cornea receives its nourishment from the tears and aqueous humor that fills the chamber behind it. To see well, all layers of the cornea must be free of any cloudy or opaque areas. When cornea becomes cloudy due to disease, injury, infection or malnutrition, vision is significantly lost or reduced.
Cornea Transplantation :
Are You a Cornea Transplant Candidate?
- Scarring from infections such as eye herpes, fungal or bacterial Keratitis.
- Hereditary corneal diseases or dystrophies.
- Thinning of cornea or irregular shape due to Keratoconus.
- Chemical burns on the cornea.
- Excessive swelling on the cornea.
Procedure for Cornea Transplant
- Registeration for cornea transplant would be done after consultation with your cornea surgeon.
- The waiting period for a donor eye depends on the voluntary donation of the eye, thus the waiting period may vary.
Refractive errors: If the cornea is flatter than normal or the eye is short, rays of light are focused behind the retina and causes hyperopia or farsightedness where close objects appear blurred.
Astigmatism is a condition in which the uneven curvature of the cornea blurs and distorts both distant and near objects. The cornea is more curved in one direction than in the other. This causes the rays of light to focus on two separate areas of the retina, distorting the visual image.
Refractive errors are usually corrected by eye glasses or contact lenses. Although these are safe and effective methods for treating refractive errors, refractive surgeries are becoming an increasingly popular option.
Allergies: Allergies affecting the eye are relatively common. They are most commonly related to pollen and dust in the air. They are usually immediate or delayed hypersensitivity reactions. Symptoms can include redness, itching, and burning, tearing, stinging and watery discharge. An increasing number of eye allergy cases are related to medications and contact lens wear.
Conjunctivitis (red / pink eye): Conjunctiva is a translucent mucous membrane which lines the posterior surface of the eyelids and anterior aspect of the eyeball. A group of diseases that cause swelling, itching, burning and redness of the conjunctiva are termed as conjunctivitis. It is an inflammation of the conjunctiva associated with a discharge which may be watery, mucoid, mucopurulent or purulent. It can spread from one person to another if proper precautions are not taken.
Infections: A breach in the normal epithelial surface of the cornea associated with necrosis of surrounding corneal tissue is termed as corneal ulceration. Two main factors are responsible in the production of a corneal ulcer: damage to corneal epithelium and infection of the eroded area. They usually cause pain, redness, watering, discharge, photophobia i.e. intolerance to light and blurred vision. It can be caused by bacteria, fungi, viruses, acanthamoeba and many other organisms.
Dry Eye: Dry eye can be caused due to any of the following reasons:
- Aqueous tear deficiency
- Mucin deficiency
- Lipid deficiency
- Impaired eyelid function
- Corneal epithelium abnormalities
Dystrophies: Corneal dystrophies affect vision in widely differing ways. Some cause severe visual impairment, while a few cause no vision problems and are discovered during a routine eye examination. Other dystrophies may cause repeated episodes of pain without leading to permanent loss of vision.
Keratoconus: Keratoconus is characterized by progressive thinning and ectasia which results in deterioration of the quality of vision and also the quality of life. A new modality of treatment, based on collagen crosslinking with the help of Ultraviolet A (UVA, 365nm) and the photosensitizer riboflavin phosphate has been described which changes the intrinsic biomechanical properties of the cornea, increasing its strength by almost 300%.
Pterygium: Pterygia are more common in sunny climates and in the 20-40 age group. Scientists do not know what causes pterygia to develop. However, since people who have pterygia usually have spent a significant time outdoors, many doctors believe ultraviolet (UV) light from the sun may be a factor. In areas where sunlight is strong, wearing protective eyeglasses, sunglasses, and/or hats with brims are suggested. While some studies report a higher prevalence of pterygia in men than in women, this may reflect different rates of exposure to UV light.
Ocular surface problems: Patients with ocular surface diseases suffer from loss of vision, discomfort, infection, erosions, ulceration, and destruction with scarring of the eye surface. The most common cause of these problems is the imbalance in the neural regulation which leads to an “unstable tear film”. Ocular surface failure manifests in two ways – the first one is the Limbal Stem Cell Deficiency in which the corneal epithelium is replaced by the conjunctival epithelium. In the second one, the corneal or the conjunctival epithelium changes with keratinisation and loss of mucosal epithelial characteristics.
Contact lens related problems: A contact lens wearer who presents with conjunctival irritation and associated symptoms – such as itching, burning or tearing – may be suffering from any one of a number of conditions (such as allergy) of which the lenses may not be the primary cause. In other cases, however, contact lens wear itself is responsible for the condition.
Aphakic /pseudophakic bullous keratopathy
- Aqueous tear deficiency
- Mucin deficiency
- Lipid deficiency
- Impaired eyelid function
- Corneal epithelium abnormalities